A recent study led by the University of Surrey has achieved a significant milestone in tuberculosis (TB) treatment monitoring by detecting antibiotics in fingerprint sweat with near-comparable accuracy to traditional blood tests.
Tuberculosis remains one of the top infectious disease killers worldwide, causing an estimated 1.3 million deaths in 2022 alone. While drug-susceptible TB is curable, patient adherence to the lengthy antibiotic regimen is crucial. Approximately half of TB patients do not adhere fully to their prescribed treatment, risking the development of drug-resistant TB strains.
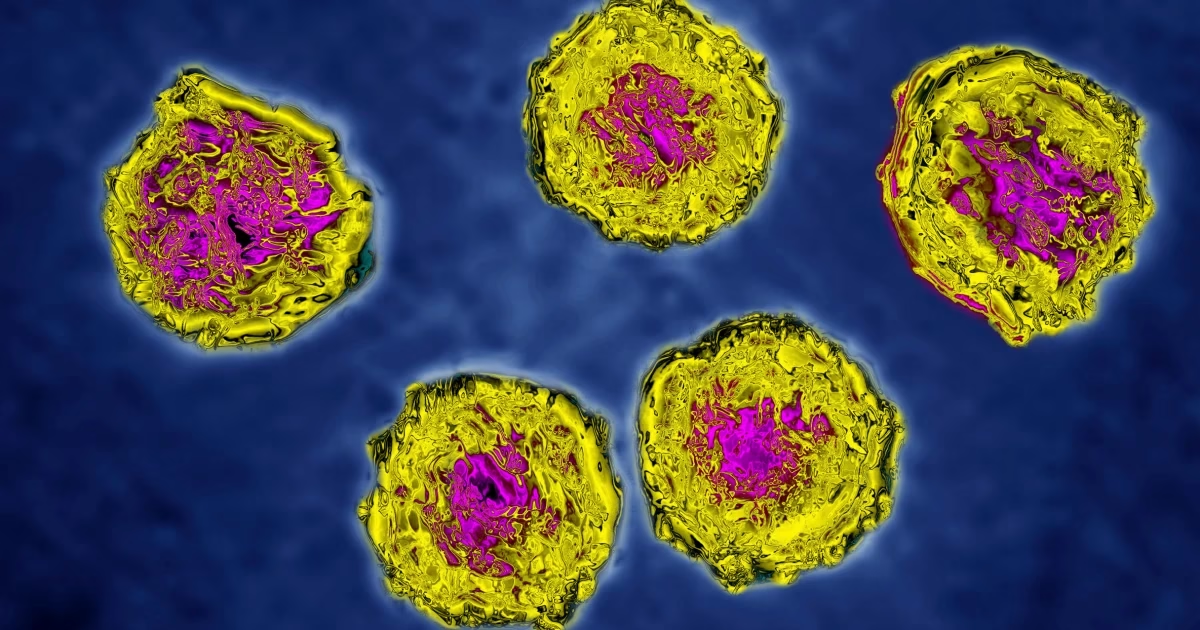
To address this challenge, researchers at the University of Surrey explored a non-invasive and painless method to monitor antibiotic levels in patients’ bloodstream. Drawing from their expertise in forensic science, where fingerprint analysis is routine, the team investigated the chemical composition of fingerprint sweat as a potential biomarker for drug presence.
Professor Bailey, leading the study, explained that fingerprints offer a convenient sample for clinical testing, devoid of the discomfort associated with blood draws. During the COVID-19 pandemic, when collecting blood and saliva samples was challenging, collecting sweat proved consistently feasible and non-invasive.
In collaboration with the University Medical Center Groningen in the Netherlands, the team tested their method on a sample group of ten TB patients. By inducing sweat with a nitrile glove and collecting it on paper squares, they successfully detected antibiotics and their metabolites with impressive accuracy: 96% for antibiotics and 77% for metabolites. The optimal detection window ranged from one to six hours post-drug ingestion.
Dr. Onno Akkerman from UMCG emphasized the simplicity of the procedure, highlighting its potential utility in routine clinical settings. This approach not only provides rapid feedback on antibiotic adherence but also avoids the biohazard concerns associated with blood sampling.
Dr. Katie Longman, co-author of the study, underscored the practical advantages of using fingerprint sweat over blood tests in monitoring TB treatment. The method offers a quicker, more comfortable alternative for both patients and healthcare providers, potentially easing the burden on healthcare systems.
Moving forward, this innovative technique holds promise for enhancing treatment adherence monitoring in TB and possibly other infectious diseases, offering a paradigm shift towards more patient-friendly and efficient healthcare practices.
This breakthrough study, published recently, marks a significant step towards personalized medicine and improved outcomes in global TB control efforts.